[objective] To report three cases of worsening glucose tolerance patients with lamivudine (3TC) therapy for hepatitis B virus.
[Introduction] Lamivudine (3TC) , a n nucleotide reverse
transcriptase inhibitor (NRTI), was screened for a drug to treat human immunodeficiency virus (HIV) infection in 1989. 3TC's clinical use was started in 1990 for HIV-infected patients. Hepatitis B virus (HBV) also needs reverse transcription in the process of its proliferation. From 2000, the 3TC therapy was started for HBV infection in Japan. In medication of HIV with 3TC, a few cases of lactic acidosis or ketoacidosis were reported. A clinical trial of AZT (400 mg per day) and 3TC (300 mg per day) for HIV carriers showed 6 hyperglycemia cases among 42 HIV-infected cases in Japan. In the trial for HBV therapy with 3TC (100 mg per day), 17 cases showed newly positive urinary glucose among 345 cases.
Kakuda reported the NRTIs inhibit mitochondrial DNA polymerase gamma.
The mitochondrial enzymes adenylate kinase and the adenosine
diphosphate/adenosine triphosphate translocator are also impaired. These mitochondrial toxicity are thought leading to the diabetes, ototoxicity, pancreatitis and multiple symmetric lipomatosis. Those long-term adverse effects are seen commonly in highly active antiretroviral therapy (HAART) for HIV-infected patients.
We report three cases of worsening glucose tolerance patients with 3TC therapy for hepatitis B virus and discuss the mechanism of glucose intolerance.
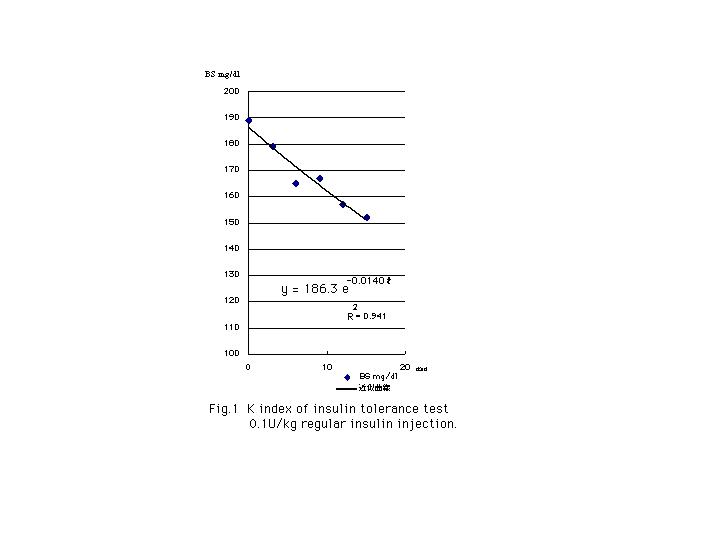
[Methods] We investigate the insulin resistance in Case 1) with the K index of insulin tolerance test (KITT) and the steady state plasma glucose level (SSPG). In KITT, we measured blood glucose before and after injection of 0.1u regular insulin / kg and 10 cc saline intravenously, every 3 minutes to 15 minutes. With Microsoft Excels (Seattle Washington USA), we plotted the approximate exponential disappearance curve and estimated the K index and half-time of blood glucose.
In SSPG, after bolus injection of 7.5 mU/kg regular insulin, we dripped 6 mg/kg/min. of glucose, 0.77 mU/ kg/min. of regular insulin and 150 micro g/body/2 hr of octeroid acetate for 120 minuets. We measured blood glucose and serum insulin levels at 0, 60, 90 and 120 minutes. The average glucose level of 60, 90 and 120 minutes is SSPG (mg/dl). Mean KITT level is 5 % / min. and SSPG of untreated diabetic patients is 185mg/dl.
We investigate the insulin resistance in Case 2) with HOMA-IR and sigma IRI. The patient was examined 75g oral glucose tolerance test (OGTT) and measured IRI (micro u / ml) and blood glucose (mg/dl). HOMA-IR was calculated IRI x BS / 405. Sigma IRI was sum of IRI at 0, 30, 60, 90, 120 and 180 min. Insulin resistance was shown if HOMA-IR is over 3.0 (10^-4 *micro u * mg * L^-2) and / or sigma IRI is over 300 (micro u / ml). The HOMA-IR are 1.56 +/- 1.12 among normal glucose tolerance cases, 2.38 +/- 1.66 among inpaired glucose tolerance cases and 3.94 +/- 2.52 among non-treated diabetic cases. In 100 g OGTT cases , sigma IRI is 268+/- 149 micro U / ml among normal glucose tolerance, 331 +/- 201 micro U / ml among inpaired glucose tolerance and 181 +/- 107 micro U / ml among non treated diabetic cases.
We examined the ability of endogenous insulin secretion in Case 3) with glucagon injection test. 1 mg of glucagon was injected intravenously and measured serum C-peptide (ng/ml).
[Case presentation]
#case 1); A 33 years-old-male was presented blood glucose 633 mg/dl, total keton 625 micro mol / L, lactic acid 11.3 mg/dl and arterial pH 7.38 at 24 July 2002. He felt fatigue and lost his weight about -10 kg from 80 kg(body mass index (BMI); 27.0 kg*m^-2) to 68.95 kg (BMI; 24.0 kg*m^-2) after he started 3TC (100 mg per day) therapy for recrudescence of HBV inflammation at 1 March 2002.
His fasting blood glucose was between 80~97 mg/dl and random blood glucose was between 162~191 mg/dl before 3TC therapy. And random blood glucose were worsen 290 mg/dl at 15 May 2002, 353 mg/dl at 19 June 2002.
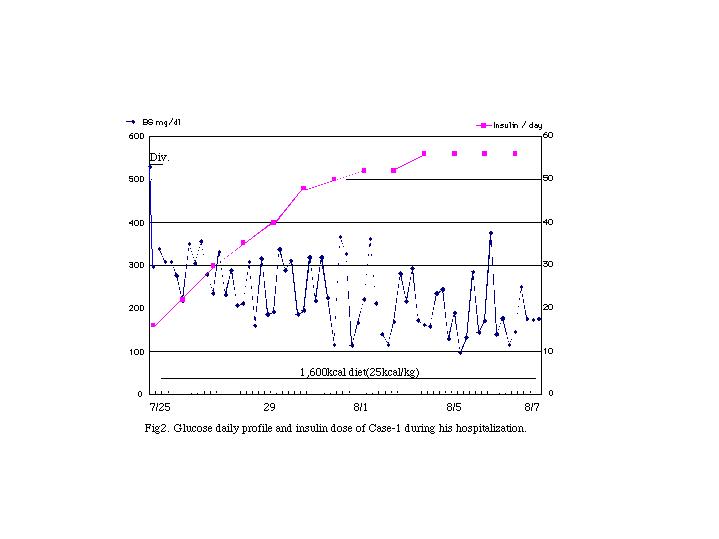
After his admission we kept saline line. The next day, we started multiple insulin injection of regular insulin 16 unit per day and 1600 kcal diet therapy. We did not stop 3TC, because we are afraid of remission of hepatitis.
He showed moderate insulin resistance, SSPG is 313 mg/dl and KITT is 1.4% / min. Half-time of glucose after 0.1u/kg insulin tolerance test was 49.5 min. He needed 56 unit insulin per day ; 0.8 unit /kg per day.
But, his ability of endogenous insulin secretion is residual. His urine C-peptide was between 40 ~ 50 micro g per day and his serum C peptide was 4.10 ng/ml at admission and 3.44 ng/ml before his discharge. His anti GAD Ab was negative. His audiogram did not show deafness ( right 6.3 dB, left10.0 dB ).
# case 2); A 48 years-old-male was presented positive urine glucose after he started 3TC (100 mg per day) therapy for HBV inflammation recrudescence at 9 Dec 2000. At 14 Feb. 2001, his random blood glucose was 240 mg/dl. He was told diet therapy from his physician ( daily intake was not shown) and decreased his blood glucose between 120~140 mg/dl in spring.
But his glucose tolerance was worsen in summer. In August, 75 g OGTT was examined and he had insulin resistance, Sigma IRI was 367 micro U/ml and HOMA-IR was 4.9. He was taught 1600 kcal diet therapy and lost his weight from 65 kg (BMI; 23.8 kg*m^-2) to 55 kg (BMI; 20.2 kg*m^-2) until summer 2002. His glucose tolerance has gotten better, his HbA1c is between 4.2~ 5.0% and FBS is between 82~118 mg/dl.
We did not stop 3TC, because we are afraid of remission of hepatitis.
He manifested proteinuria before, 0.71 g per day at 4 July 2001. But, urine protein was decreased 0.18 g per day until 21 Nov. 2001. Proteinuria is now disappeared in test tape .
# case 3 ); A 77 years-old-male has been pointed out type 2 diabetes and chronic hepatitis due to HBV. His HbA1c was between 7.2 ~ 7.3% with 1600 ~ 1800 kcal diet therapy. In Oct. 2001, ascites was pointed out in abdominal ultra sound echogram. After admission in Nov. 2001, he started 3TC therapy. His HBV-DNA decreased from 8.3 Leg copy per ml to under 3.7 Leg copy / ml and his ascites was disappeared. His FBS was slightly worsen from 115 mg/dl at admission to 136 mg/dl at discharge. In out patient's clinic visit, his random blood glucose was increased to 363 mg/dl at Feb. and to 463 mg/dl at Mar.
He was hospitalized at 24 May. At admission, FBS was 185 mg/dl and HbA1c was 10.7%. We started multiple regular insulin injection therapy from 12 unit per day to 19 unit per day. His FBS was decreased to 128 mg/dl at discharges. Before his discharge, we examined residual ability of endogenous insulin secretion with 1 mg glucagon injection test. His serum C peptide was increased from 1.47 ng/ml to 4.62 ng/ml at 6 min..
His audiogram showed mild deafness, rt. 24 dB and lt. 20 dB. But, he felt difficulty of hearing before 3TC therapy started.
[Discussion]
In these three cases, their glucose tolerance were worsen around about 3 months after 3TC therapy. In case 1) and 2), they showed moderate insulin resistance. In case 1) and 3), insulin therapy were needed to treat their glucose control. We continued 3TC therapy , because we are afraid of worsening hepatitis with stopping of 3TC.
In these three cases, insulin secretion were residual, anti GAD Ab were null and no insulin deficiency were shown. Autoimmunity and pancreatitis are not manifested among them.
One of them was presented mild hearing difficulty, but that appeared before 3TC therapy and mitochondrial toxicity is not confirmed. The deafness in case 3) might be due to his age.
We thought the appearance of insulin resistance might occur their glucose intolerance. We concerned the use of thiazolidinediones or biguanides, but either drugs have the adverse effect of liver dysfunction.
In their history, they said no increase of their food or soft-drink intake. But, like the cases of olamzapines, better general condition can increased their intake calories and might worsen their glucose tolerance.
In trials among Japanese HIV or HBV patients, 3TC are suspected to worsen glucose tolerance. But, in the examination at Europe and North America, HIV patients are administrated HAART, patients are also given protease inhibitors (PI) .
In the Mulligan's study of lipoatrophy during HAART, PIs represented insulin resistance, fasting IRI increased +12.2+/-4.9 micro U/ml; p = .023 and FBS increased +9+/-3 mg/dl; p = .0136. But, there is no difference among the control groups and NRTI groups.
Carr said that NRTIs showed increased lactic acid and transaminase and PIs showed increased blood glucose and fasting insulin. Among HAART therapy, three patients showed severe hyperglycemia with acidosis, either lactic or ketotic. All cases showed strong insulin resistance. All three cases used both NRTIs and PIs, all authors concerned that PIs rolled major places in their manifestation of glucose intolerance.
In case of #2 , proteinuria disappeared during 3TC therapy. Al Faraidy mentioned the utility of 3TC among patients of HBV related nephropathy.
[Conclusion]
3TC therapy for HBV are utility, but it can occur glucose intolerance in some cases. We must concern the possibility of worsening glucose controls after 3TC therapy among HBV patients.
The most possible mechanism of hyperglycemia might be insulin resistance. The prospective study for insulin sensitivity after 3TC therapy is needed for making clear answer in this problem.