[-> contents]
[ Document Identification Number : DIN01022812 ]
Digital Color Imaging in Biomedicine (in press), 2001.02.28 (draft)
<http://biocolor.umin.ac.jp/book200102/din01022812.pdf>
Digital Color Imaging in Biomedicine (in press), 2001.02.28 (draft)
<http://biocolor.umin.ac.jp/book200102/din01022812.pdf>
|
From the Standpoint of Dermatology
Toshihiko NUMAHARA*1 (numahara@kms.ac.jp) *1Department of Dermatology, Kagawa Medical University |
|
Abstract: Because skin color directly reflects every pathological change of skin that causes modification of its optical characteristics, it is vital information in dermatological diagnosis. Photographs have played a substantial role for a long time in recording skin lesions, and recently digital imaging has been introduced for this purpose. But the quality of skin color images reproduced by any current imaging system does not meet the requirement for dermatological diagnosis, therefore they are not yet considered a substitute for the observation of the real objects and only subsidiary roles are given to them.
However, if advanced digital imaging technologies including multispectral imaging are in a position to reproduce images which can be equally used as real objects, revolutionary changes are expected in dermatological practice as well as in dermatological education. If, on the other hand, the technology of digital imaging fails to achieve higher quality as mentioned above, a huge investment in electronic patient records and tele-medicine would run the risk of having been made in vain in the field of dermatology. |
|
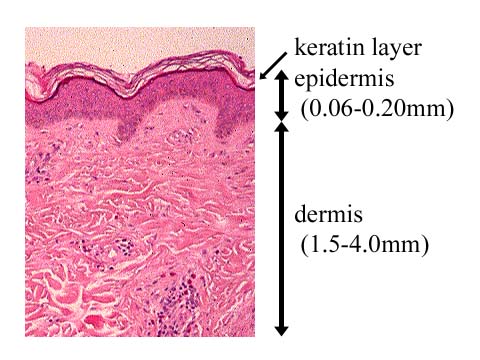
1. Understanding human skin and its color 1.1 The structure of human skin (Fig. 1) The thickness of human skin except for subcutaneous tissue varies from 1.5 mm to 4.0 mm according to age, sex or body regions. The most superficial layer of the epidermis is the keratin layer, which is 0.02 mm thick generally and 0.5 mm thick at the palms and soles of the feet. The epidermis has melanocytes in a 10 percent ratio of all cells in its basal layer and they supply melanin to keratinocytes. This melanin plays a great role in protecting the skin from the harmful effects of ultraviolet light. In the dermis, the papillary layer just under the epidermis is rich both in capillaries and in the terminal organs of sensory nerves, and the reticular layer that accounts for the most part of the dermis is rich in collagenic fibers. |
|
|
 |
|
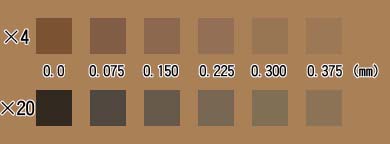
1.2 The origins of skin colors [1-3] Roughly speaking, illuminated light which comes into the skin is scattered in the dermis and a part of it is absorbed by melanin and hemoglobin, then the rest of the light makes the familiar flesh color (Fig. 2). Increased melanin in the epidermis intensifies the brownish tone of the skin color, and dilated vessels in the inflamed skin cause a more reddish tone of skin color (Fig. 3). Also, other pigments such as bilirubin and carotene in plasma as well as changes in the optical characteristics of the keratin layer or of the dermis have considerable influence on skin color. For example, if the keratin layer s thicker or dry, more light is scattered and consequently the skin increases its opacity (Fig. 4). |
|
|
 |
|
|
 |
|
|
 |
|
The dermis is often compared to agar containing milk because it requires a certain thickness to appear to be white. Its pathological changes such as atrophy, degeneration and edema cause modification of its optical characteristics and consequently make up the changes in skin color. In the dermis, light of a longer wavelength (red light) penetrates it more easily than a shorter one, and contrary, light of shorter wavelength (blue light) is more scattered than a longer one. When there is a substantial amount of pigment in the deep layer of the dermis, a larger amount of light of a shorter wavelength, which tends to be scattered in the superficial layer, reaches observers' eyes than light of longer wavelength, which tends to penetrate the dermis and be absorbed by the pigment in it. This is the reason why dilated capillaries and strawberry marks in a superficial layer of skin look vivid and deep red and, on the other hand, veins and hemangiomas in a deeper layer look bluish. In the same way, junction nevi made of melanocytes situated at the boundary between the dermis and the epidermis look brownish, but blue nevi situated in the dermis look bluish as its name indicates, and nevi of Ota and Mongolian spots, both of which are made of dermal melanocytes, also look bluish (Fig. 5). |
|
|
 |
|
2. Skin color and dermatological diagnosis In dermatology, because the macroscopic pathology of lesions is directly observed and used to evaluate their microscopic changes, visual findings are essential for diagnosis. Dermatological findings include major skin signs of the lesions: (1) type, (2) shape, (3) arrangement and (4) distribution, and especially skin color is vital information for interpreting the characteristics of lesions and the depth at which they exist in the skin (Fig. 6). Therefore various terms including white, red, pink, violaceous, brown, black, blue, gray, orange, yellow, etc. and more delicate ones, for example, salmon pink, slate, cafe au lait, black pearl, heliotrope and waxy are used to describe the colors of skin lesions. Among the colors seen in various skin diseases, the diagnostic importance of red in immunologic and inflammatory disorders is larger than in proliferate and neoplastic ones (Fig. 7). Deep red reflects severe inflammation, vivid red reflects an acute condition and purplish red reflects damage in the basic layer of the epidermis. |
|
|
 |
|
|
 |
|
3. Visual records of skin lesions In dermatology, visual recording of skin lesions is extremely important. Its long history has centuries of precise sketches, nearly a century of moulages, which are lifelike models of simulated shapes and colors of skin lesions, and thereafter decades of 35 mm photographs, which have long been considered to be the de facto standard. Nevertheless, these technologies are not considered to be able to substitute for observing the real objects because of limitations in their fidelity and durability. Therefore expenses for these processes are not reimbursed by medical insurance in Japan. 4. Digital imaging required for dermatological diagnosis The recent progress and rapid spread of digital imaging technologies have brought digital cameras and desktop computers equipped with handy image processing software into medical practice. In dermatology, they are required to record accurate skin colors, especially fine red colors, and to reproduce them, but there is an extremely wide range of variation, not only among healthy and diseased skin, but also among the racial skin differences of caucasian, Asian and black individuals. In reality, there are severe limitations and large differences in the colors reproduced by the various equipment used for digital imaging, which may incidentally cause erroneous diagnoses (Fig. 8). The author experienced serious problems of this kind in publishing a CD-ROM based color atlas instructing dermatological diagnosis [4]. |
|
|
 |
|
If digital imaging technology stays in the present state and does not achieve the quality required, then a huge investment made in electronic patient records and tele-medicine would run the risk of having been made in vain in the field of dermatology.
Contrary, if advanced digital imaging technologies can reproduce images which can be equally used as real objects for dermatological diagnosis, revolutionary changes in medicine may be expected. Precise dermatological findings are conveyed when a patient is introduced to a distant physician or a medical consultation is made with a distant specialist. In addition, the importance of morphological records in dermatological practice as well as in dermatological education will be extremely increased. 5. Conclusions Accurate color reproduction in digital imaging is one of the vital issues in dermatology of 21st century, therefore research activities like this symposium focused on it are expected to evolve further and to play important roles in establishing new and effective standards based on highly advanced imaging technologies, including multispectral imaging, to solve the emerging color problems confronting us. Acknowledgments I am grateful to Dr. Hirotsugu Takiwaki (Department of Dermatology, Tokushima University, Japan) for kindly providing me with his valuable simulating software and related literature. References
|